Telehealth Mental Health Services: 15% Growth & 2025 Accessibility

The 15% increase in telehealth mental health services is transforming healthcare delivery, making professional support more readily available and significantly improving accessibility for diverse populations across the United States by 2025.
The landscape of mental healthcare is experiencing a profound transformation, with a notable 15% increase in telehealth mental health services. This surge isn’t just a statistic; it represents a fundamental shift in how individuals access vital support, promising enhanced accessibility and evolving care models by 2025. What does this growth truly signify for the future of mental wellness?
The rise of telehealth in mental wellness
Telehealth has rapidly moved from a niche solution to a mainstream component of healthcare delivery, particularly within mental wellness. The convenience and flexibility it offers have resonated deeply with both providers and patients, accelerating its adoption rates across the United States.
This expansion is not accidental; it is driven by several converging factors, including technological advancements, evolving patient preferences, and policy changes that have supported its integration. The ability to connect with a therapist or psychiatrist from the comfort of one’s home has removed numerous barriers that traditionally hindered access to mental health support.
Overcoming geographical barriers
For many years, individuals in rural areas or those without reliable transportation faced significant challenges in accessing mental health professionals. Telehealth effectively bridges these geographical gaps, bringing expert care directly to patients, regardless of their location.
- Reduced travel time and costs for patients.
- Access to specialists not available locally.
- Greater choice of providers across state lines (where licensed).
The impact of this increased reach cannot be overstated. It ensures that mental health support is not a luxury reserved for urban dwellers but a fundamental right accessible to everyone, fostering a more equitable healthcare system.
Addressing stigma and privacy concerns
Mental health conditions often carry a societal stigma, which can deter individuals from seeking help. Telehealth offers a discreet way to engage with therapists, reducing the anxiety associated with visiting a physical office.
The privacy of a home setting can make patients feel more comfortable and open during sessions, leading to more productive therapeutic outcomes. This element of discretion is a powerful tool in breaking down the barriers of shame and judgment that often accompany mental health struggles.
Understanding the 15% increase: what’s driving it?
The reported 15% increase in telehealth mental health services is a clear indicator of a significant shift in healthcare delivery. This growth is multifaceted, stemming from various factors that have converged to make virtual care a preferred option for many.
One of the primary drivers is the sheer convenience it offers. Patients can schedule appointments around their work, family, and personal commitments without the added stress of commuting or taking time off. This flexibility is invaluable for busy individuals who might otherwise postpone or forgo therapy.
Technological advancements and platform maturity
The rapid evolution of communication technologies has played a crucial role. High-speed internet access is more widespread, and telehealth platforms have become more robust, user-friendly, and secure. These platforms now offer features like virtual waiting rooms, secure messaging, and integrated payment systems, enhancing the overall patient experience.
- Improved video and audio quality for seamless sessions.
- Enhanced data security and HIPAA compliance.
- Integration with electronic health records (EHRs).
The reliability of these technologies means that virtual sessions are often as effective as in-person ones, fostering trust and encouraging continued use.
Policy changes and insurance coverage
Government policies and insurance companies have increasingly recognized the value and efficacy of telehealth. During the pandemic, many regulatory barriers were temporarily lifted, and insurance coverage expanded significantly. These changes have largely remained in place, solidifying telehealth’s position in the healthcare ecosystem.
Insurance parity laws, which mandate that telehealth services be reimbursed at the same rate as in-person services, have been instrumental in encouraging providers to adopt virtual care models. This financial incentive, coupled with a growing demand from patients, has created a fertile ground for telehealth expansion.
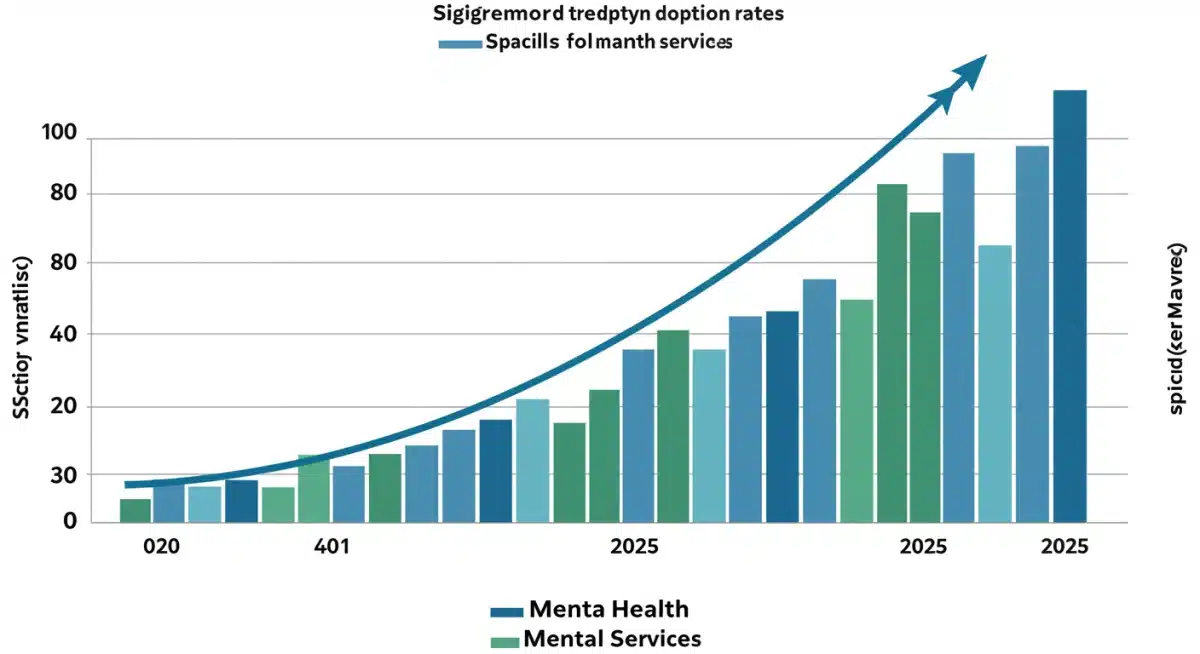
Accessibility in 2025: a new paradigm
By 2025, the impact of the 15% increase in telehealth mental health services is expected to usher in a new paradigm of accessibility. This isn’t merely about more available appointments; it’s about fundamentally reshaping who can access care, when, and how.
We anticipate a future where mental health support is integrated more seamlessly into daily life, becoming less of a hurdle and more of a readily available resource. This enhanced accessibility will have far-reaching implications for public health and individual well-being.
Reaching underserved populations
One of the most significant promises of telehealth is its potential to serve populations that have historically been underserved. This includes not only those in rural areas but also individuals with physical disabilities, chronic illnesses, or those who are housebound.
Telehealth removes the physical barriers that often prevent these groups from seeking care, offering a lifeline to support that was previously out of reach. It also provides a culturally sensitive option for some communities, allowing them to connect with providers who understand their unique needs and backgrounds.
Flexible scheduling and reduced wait times
The traditional mental healthcare system has often been plagued by long wait times for appointments, which can be detrimental for individuals in crisis or those needing immediate support. Telehealth offers greater flexibility in scheduling, with many platforms providing on-demand or next-day appointments.
- Extended hours for evening and weekend sessions.
- Ability to switch providers more easily if a match isn’t optimal.
- Reduced administrative burden for both patients and clinics.
This agility in scheduling means that individuals can receive timely interventions, preventing conditions from escalating and promoting earlier recovery.
Challenges and considerations for sustained growth
While the growth in telehealth mental health services is overwhelmingly positive, it is essential to acknowledge and address the challenges that could impact its sustained expansion. Ensuring equitable and effective care requires continuous effort and adaptation.
One significant concern is the digital divide. Not everyone has reliable access to high-speed internet or the necessary devices, which can exclude certain segments of the population from benefiting from telehealth. Bridging this gap is crucial for true universal accessibility.
Ensuring quality and continuity of care
Maintaining the quality and continuity of care in a virtual setting is paramount. Providers need adequate training in telehealth best practices, and platforms must facilitate seamless communication and record-keeping. The therapeutic relationship, a cornerstone of mental health treatment, must be effectively fostered remotely.
- Standardized training for telehealth providers.
- Robust protocols for crisis intervention in a virtual setting.
- Interoperability between telehealth platforms and EHRs.
Regular assessments of patient outcomes and satisfaction are also vital to ensure that telehealth remains an effective mode of treatment.
Regulatory landscape and interstate licensing
The regulatory environment for telehealth is still evolving, particularly regarding interstate licensing. While some temporary waivers were enacted during the pandemic, a more permanent and streamlined approach is needed to allow providers to serve patients across state lines efficiently.
Clarity on reimbursement policies, data privacy regulations, and ethical guidelines for virtual care will be essential for creating a stable and predictable environment for continued growth. Advocacy for supportive legislation is ongoing and critical for the future of telehealth.
The impact on mental health professionals
The surge in telehealth mental health services also has significant implications for mental health professionals. While it offers new opportunities, it also presents unique challenges and requires adaptation from practitioners.
Many therapists and psychiatrists have embraced telehealth, finding it allows for greater flexibility in their own schedules and expands their client base. It can reduce overhead costs associated with maintaining a physical office, potentially making private practice more accessible.
Training and adaptation for virtual practice
For some professionals, transitioning to virtual care requires new skills and training. This includes mastering telehealth technology, adapting therapeutic techniques for a screen-based environment, and understanding the nuances of remote client engagement.
- Developing strong virtual rapport with clients.
- Utilizing digital tools for therapeutic exercises.
- Managing technical issues during sessions.
Professional organizations and educational institutions are increasingly offering specialized training programs to equip clinicians with the competencies needed for effective telehealth practice.
Preventing burnout and promoting well-being
While telehealth offers flexibility, it can also contribute to provider burnout if not managed effectively. The constant screen time and the intensity of mental health work can be draining. It’s crucial for professionals to establish boundaries and engage in self-care practices.
Support networks for telehealth providers, peer supervision, and access to their own mental health support are vital to ensure the long-term sustainability of the workforce and the quality of care they provide.
Future outlook: telehealth as a cornerstone of care
Looking towards 2025 and beyond, it is clear that telehealth mental health services are not a temporary trend but a fundamental shift in how we approach mental wellness. The 15% increase is just the beginning of a sustained integration into the broader healthcare system.
We can expect further innovation in telehealth technology, with the potential for virtual reality and artificial intelligence to enhance therapeutic interventions. The focus will increasingly be on personalized care, leveraging data to tailor treatments to individual needs.
Integrated care models
Telehealth facilitates the integration of mental health care with primary care and other medical specialties. This holistic approach ensures that mental health is not treated in isolation but as an essential component of overall health and well-being.
For example, a primary care physician might easily refer a patient to a telehealth therapist, with both providers having access to relevant patient information (with consent). This collaborative model can lead to more comprehensive and coordinated care.
Preventive and proactive mental health
With greater accessibility, telehealth can shift the focus from reactive treatment to proactive and preventive mental health. Easier access to early intervention can help individuals manage stress, anxiety, and other conditions before they escalate.
- Increased access to mental health screenings.
- Online resources for self-help and psychoeducation.
- Community-based telehealth programs.
This proactive approach can lead to improved population-level mental health outcomes, fostering a more resilient and mentally healthy society.
| Key Aspect | Brief Description |
|---|---|
| 15% Growth Drivers | Increased convenience, technological advancements, and supportive policy changes are fueling the surge in telehealth mental health services. |
| Enhanced Accessibility | Telehealth breaks down geographical barriers and addresses stigma, making mental health support available to more people, especially underserved populations. |
| 2025 Outlook | By 2025, telehealth is expected to be a cornerstone of mental healthcare, integrating care and promoting proactive mental wellness strategies. |
| Key Challenges | Addressing the digital divide, ensuring quality of care, and navigating evolving regulations are crucial for sustained growth. |
Frequently asked questions about telehealth mental health
The increase is primarily driven by enhanced convenience, significant technological advancements making platforms more user-friendly, and supportive policy changes including expanded insurance coverage that incentivizes virtual care for both patients and providers.
Telehealth improves accessibility by removing geographical barriers, reducing travel time, offering flexible scheduling, and providing a discreet way to seek help, which can significantly reduce the stigma often associated with mental health treatment.
Key challenges include bridging the digital divide to ensure equitable access, maintaining the quality and continuity of care in a virtual setting, and navigating the complex and evolving regulatory landscape, especially concerning interstate licensing and reimbursement.
While telehealth is rapidly expanding, it is more likely to complement rather than entirely replace traditional in-person therapy. Many individuals still prefer face-to-face interactions, and some complex cases might require in-person assessments. It offers a valuable alternative and expansion of care.
Telehealth offers professionals greater flexibility in their schedules, reduced overhead costs, and the ability to expand their client base beyond geographical limitations. It also supports work-life balance, though it requires adaptation to new technologies and virtual therapeutic techniques.
Conclusion
The 15% increase in telehealth mental health services represents a monumental step forward in making mental wellness accessible to a broader population. As we approach 2025, this trend is poised to solidify telehealth’s role as an indispensable component of the healthcare system. While challenges remain, the commitment to innovation, equitable access, and quality care will ensure that virtual mental health support continues to grow, fostering a healthier and more connected society.